Nearly every day for the past month Roxana Mehran, an interventional cardiologist at Mount Sinai Hospital in New York City, and her colleagues have been getting calls from patients wondering if their stents were really necessary.
Yes, the doctor assures them, they were prime candidates to receive a stent, a small device used to prop open clogged arteries in patients with cardiovascular disease.
Dr. Mehran, who is chair of the American College of Cardiology’s Interventional Council, says she told one such patient, “Don’t worry, I made sure with the physiology test. You were having three to four episodes of chest pain a week. You couldn’t walk two blocks.”
A study in the journal the Lancet in November has fueled an already contentious debate within cardiology over which patients really need stents. Doctors are far from a consensus on the matter. Lost in the fray: confused and concerned patients.
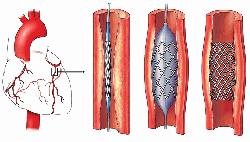
Stents are implanted during angioplasty procedures called percutaneous coronary interventions, or PCIs. Over one million stents were implanted in US patients last year, according to the American College of Cardiology’s national registry of heart catheterization facilities, which encompasses about 85% of facilities in the US.
Most cardiologists agree that in patients with acute coronary syndrome- those who have a heart attack or frequent chest pain- stents can be a lifesaver.
It’s in patients with stable angina, or chest pain that occurs only when they exert themselves that questions remain.
Some experts say a landmark 2007 New England Journal of Medicine study proved that stents don’t prevent heart attacks and death in patients with stable coronary artery disease.
The 2,287 patient study found that heart medication was just as effective as stents in preventing heart attacks and death in such patients.
The new Lancet study was conducted by researchers in the UK and was nicknamed the ORBITA trial. It found that patients with stable chest pain who received stent devices had no statistically significant improvement in their exercise time on a treadmill when compared with patients who received no stents took heart drugs for six weeks before their procedures.
Doctors perform about 500,000 PCI procedures every year world-wide on patients with stable angina, according to the study. Studies have estimated that 20% of those surgeries in the US are done on that subset of patients.
Long criticized as an overused procedure, the unnecessary insertion of stents fell by about 50% between 2010 and 2014, according to a 2015 study published in JAMA. The drop followed guidelines issued in 2009 that discouraged stent use in patients with stable disease and minimal symptoms of chest pain.
The Lancet study included only patients with one narrowed artery. Patients had chest pain symptoms for over eight months, though about 10% had no further chest pain after being treated with medication for six weeks. They were still included in the study.
Doctors perform over 20% of angioplasty procedures on US patients with stable angina who have no symptoms, says Rasha Al-Lamee, lead author of the Lancet study and an interventional cardiologist at Imperial College London.
But Dr. Mehran notes that some patients had a borderline lesion, which is an artery that is 50% to 70% blocked. “This was really a healthy patient population,” she says. “These are not the patients we see every single day.”
Ian Meredith, chief medical officer at Boston Scientific, a leading maker of stents, says that there is a wide spectrum of symptoms in patients with stable angina and that some patients can’t tolerate taking multiple heart medications.
“Certainly medications are the desired therapy for people with a low burden of symptoms and who are coping pretty well with their daily living,” he says.
Deepak L. Bhatt, executive director of interventional cardiovascular programs in the Heart & Vascular Center at Brigham and Women’s Hospital in Boston, cautions that ORBITA was a small study that shouldn’t change current clinical practice.
As to the broader question of whether too many patients are getting stents, Dr. Bhatt says if depends on which category of heart patients you look at.
“The majority of stents go in for acute coronary syndromes,” he says. “In that situation, if anything there’s an issue of patients being undertreated, especially the highest-risk patients.”
Dr. Bhatt says the use of stents for stable coronary artery disease has gone down ever since the landmark 2007 trial was published. “I don’t think there’s this vast overuse of stents,” he says. (He adds that he has no financial ties to any stent makers.)
But David Brown, a professor of medicine at Washington University School of Medicine in St. Louis, wrote a strong accompanying editorial in the Lancet saying it showed “unequivocally that there are no benefits for PCI compared with medical therapy.”
Dr. Brown hopes clinical practice will change as a result. He says most patients with stable angina likely have obstruction of their microscopic arteries, so stenting of the large vessels wouldn’t relive symptoms, reports internet.